시신경척수염 범주질환 환자의 감정실금 증례 1
Emotional Incontinence in a Patient with Neuromyelitis Optica Spectrum Disorder
Article information
Trans Abstract
The pathologic laughing is involuntary and associated with brain damage seen in a variety of disorders, which occurs as a result of lesions in various locations and is often seen associated with prefrontal or brainstem lesions. Neuromyelitis optica spectrum disorder (NMOSD) is an autoimmune inflammatory disease of the central nervous system characterized by severe attacks of optic neuritis and myelitis, and also develops brain lesions involving the bilateral diencephalic regions adjacent to the third ventricles, the brainstem and cerebellum surrounding the fourth ventricles, and the periventricular white matter adjacent to the lateral ventricles. Emotional incontinence refers to episodic laughing or crying, and occurs as a result of brain damage in various locations and is often seen associated with prefrontal or brainstem lesions. Emotional incontinence has been well described in multiple sclerosis, however the emotional incontinence in NMO has not been systemically documented. My report a characteristic patient with NMO showing the pathologic laughing as an initial manifestation, and the plasmapheresis therapy showed remarkable improvement in severity and occurrence of the pathologic laughing.
Involuntary pathologic laughing is associated with brain damage seen in a variety of disorders.1 Pathologic laughing occurs as a result of lesions in various locations and is often seen associated with prefrontal or brainstem lesions.1,2 The classical anatomic theory is suggested emphasizing the prefrontal cortex as the center integrating information from a complex emotion and sensory loop with motor information destined for the facio-respiratory nuclei in the brainstem.1,2 Disturbance at any level in the loop is proposed to produce pathologic laughing by degrading information to or from the prefrontal cortex, disrupting its inhibitory control of the nuclei. The pathologic laughing has also rarely been reported in association with brainstem stroke involving the basis pontis or the cerebral peduncles, pontine glioma, and cerebellar vermian ependymoma.1,2 And also, the emotional instability involving pathologic laughing has been described in multiple sclerosis (MS), and the prevalence of pathological laughing in MS is 10%.3 Unusually, we will describe a patient in whom pathological laughing was the symptom of neuromyelitis optica (NMO). NMO is an autoimmune inflammatory disease of the central nervous system characterized by severe attacks of optic neuritis and myelitis.4 On recent reports, some patients with NMO showed brain lesions involving the bilateral diencephalic regions adjacent to the third ventricles, the pontine tegmentum and cerebellum surrounding the fourth ventricles, and the periventricular white matter adjacent to the lateral ventricles.5 Therefore, theoretically, pathologic laughing can be found in brain lesions of NMO. However, to my knowledge, the pathologic laughing or crying in NMO has not been systemically documented. My report a patient with NMO who presented with pathologic laughing, and the treatment of the plasmapheresis showed remarkable improvement in severity and occurrence of the pathologic laughing.
Case
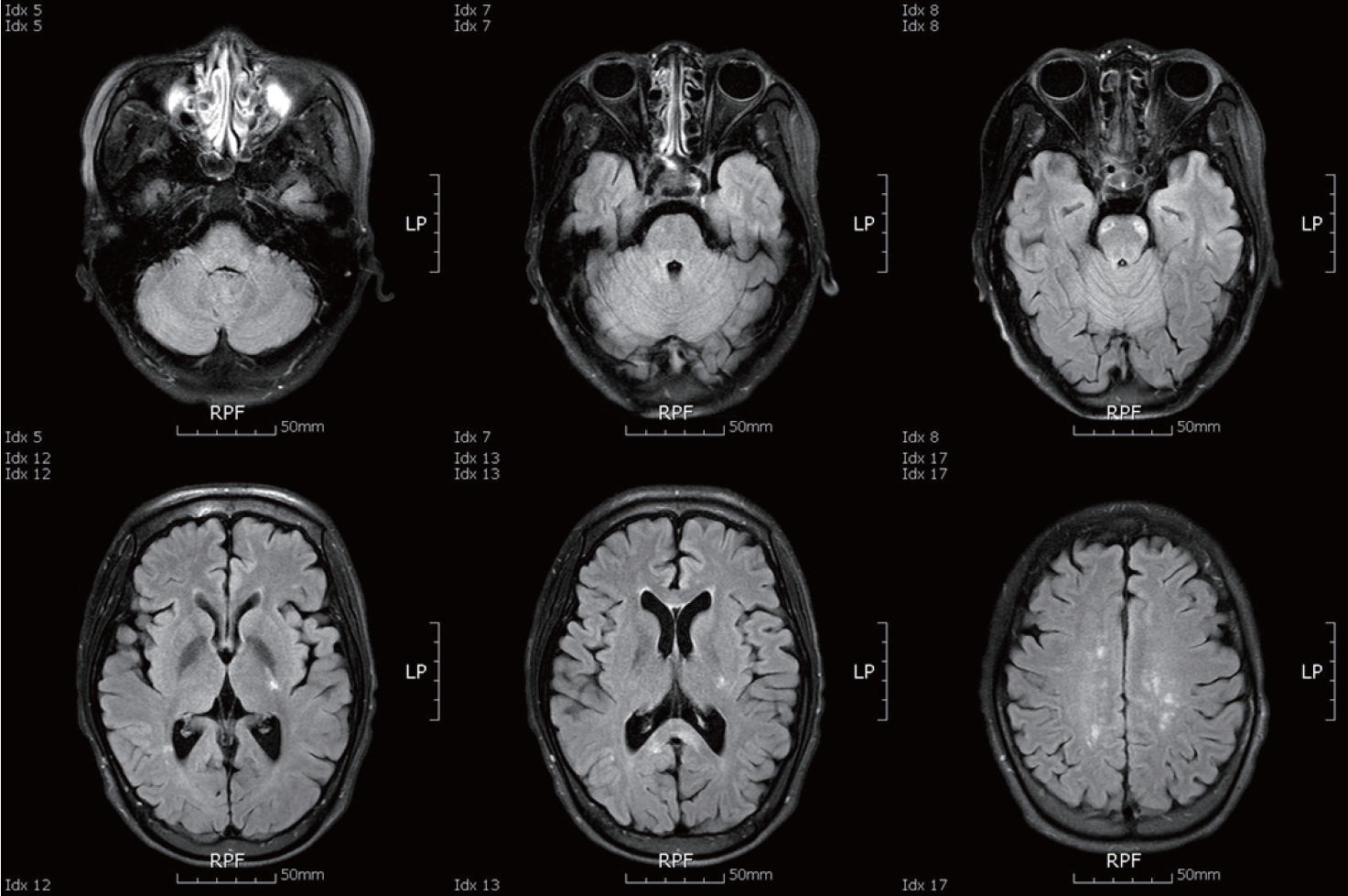
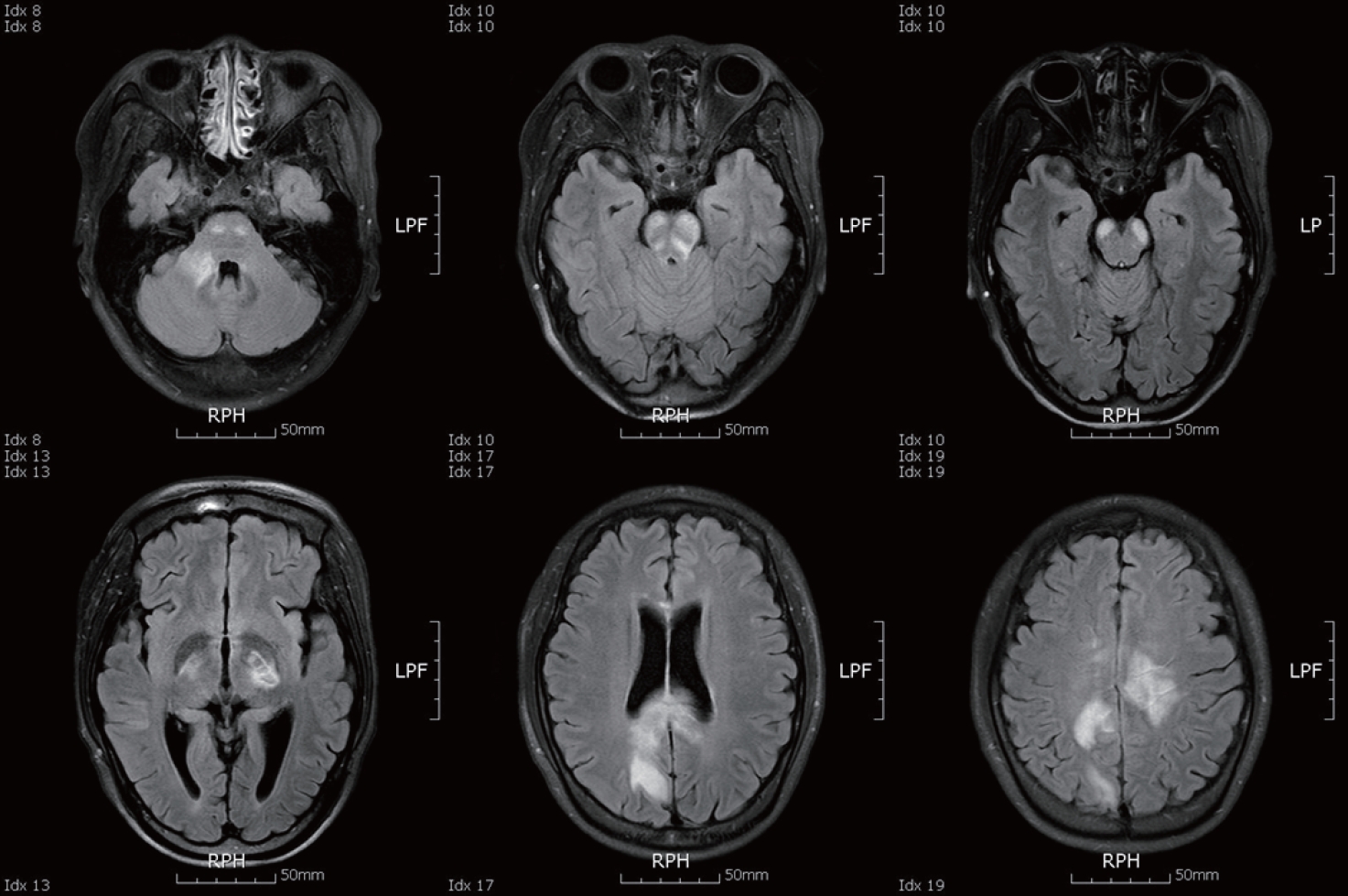
A 29-year-old woman visited my department with complaints of quadriparesis and decreased mentality. In the past medical history, since 22-year-old, she had experienced four-episode of myelitis and six-episode of optic neuritis without brain abnormality, and had been treated with oral steroid and immune-suppressants for treating the NMO. On admission, she showed a mild drowsy mentality, and neurological exam revealed severe motor weakness of Medical Research Council (MRC) grade 1 in the 4-extremities and dysarthria. In addition, interestingly, during the awakening period, she frequently laughed in response to stimuli that normally would not trigger laughing, which was consistent with pathologic laughing. Brain MRI revealed extensive lesions involving bilateral internal capsule, corpus callosum, white matters, pyramidal tract and pontomesencephalic junction of brainstem and cerebellar peduncle (Fig. 1). Cerebrospinal fluid analysis revealed increase white blood cell (120) and protein (352.8 mg/dL) without oligoclonal band. In serologic analysis, the anti-aquaporin-4 antibody was positive. Initially, the patient was initially treated for consecutive 5 days with a high dose of intravenous methylprednisolone (1 g/day), followed by a high dose of oral prednisolone (60 mg/day). In spite of the high-dose steroid therapy, her neurological symptoms did not improve. For further treatment, she was alternately treated with seven courses of plasmapheresis for 14 days. Treatment of plasmapheresis showed remarkable improvement. Her motor function improved to a MRC grade 4 after therapy of plasmapheresis, and also mentality and bulbar symptoms also improved. However, the improvement of the pathologic laughing was relatively slow compared with motor function. Even if the improvement in severity and occurrence by the plasmapheresis was significant, the pathologic laughing was sustained at 1-year follow-up. The MRI scan taken 2 months later showed regression of the initial inflammatory lesions without any new T2 lesions (Fig. 2).
Brain MRI of the patient with pathologic laughing, revealed extensive lesions involving bilateral internal capsule, corpus callosum, white matters, pyramidal tract of brainstem, pontomesencephalic area involving basis points, and cerebellar peduncle.
Discussion
NMO is an autoimmune inflammatory disease of the central nervous system characterized by severe attacks of optic neuritis and myelitis, and its definition has been documented with a revised criteria.4,5 And the discovery of a specific autoantibody against aquaporin-4 (AQP4), clinical and experimental evidence has shown that NMO has a humoral immune mechanism, and the diagnosis of NMO has evolved into a broader spectrum disorder.6,7 According to numerous reports, brain lesions in NMO are preferentially observed in regions where AQP4 is abundantly present, such as the bilateral diencephalic regions adjacent to the third ventricles, the pontine tegmentum and cerebellum surrounding the fourth ventricles, and the periventricular white matter adjacent to the lateral ventricles.5-7 My patient had recurrent optic neuritis, myelitis showing long extensive spinal cord lesion over three vertebral levels and positive AQP4 antibody, therefore she met the revised diagnostic criteria for NMO. On recent admission, my patient showed newly developed extensive lesions in the brain involving bilateral internal capsule, corpus callosum, white matters, pyramidal tract of brainstem, pontomesencephalic area of the tegmentum and cerebellar peduncle. Interestingly, my patient showed characteristic pathologic laughing during the acute stage, which was gradually resolved by the treatment of the plasmapheresis, and sustained for 1-year follow-up. To our knowledge, the case of pathologic laughing in NMO has not been systemically described, whereas the emotional instability involving pathologic laughing have been described in MS, and the prevalence of pathological laughing in MS is 10%.3,8 A recent report indicated that pathological laughing occurs in patients with severe physical disabilities, generally with longstanding disease in MS.3,8 It is also suggested pathological laughing can occur in the first attack in MS, and steroid pulse therapy treatment was effective for pathological laughing in MS. However, theoretically, pathologic laughing can be found in brain lesions of NMO, because the recent reports revealed that NMO showed brain lesions involving the brainstem, cerebellar peduncle and cerebellum surrounding the fourth ventricles. The pathophysiology of the pathological laughing is explained by the dysfunction in the cerebro-pontocerebellar pathways. The pathologic laughing has been described as not being caused by a loss of direct motor cortical inhibition of a laughing center, but rather by dysfunction in circuits that involve brainstem nuclei and the cerebellum.9,10 It was speculated that the anatomical lesion responsible for the pathological laughing is located in the pontine base, which is consistent with the inflammatory lesion in my patient.1,2,9,10 In contrast with MS, we observed improvement of the pathologic laughing in my NMO patient only after treatment by plasmapheresis. And the symptom of pathologic laughing was sustained at 1-year follow-up, which was much longer than the previous cases of MS.
Generally, the high dose-corticosteroid and plasmapheresis have been considered in an acute stage of NMO. In this case, the patient’s motor weakness and pathologic laughing did not improve in spite of consecutive high dose-corticosteroid for 2 weeks, but showed remarkable improvement after plasmapheresis therapy. My finding on the effectiveness of the plasmapheresis therapy is interesting and significant, because which indicates that the pathologic laughing of the patient with NMO will be properly treated with the plasmapheresis, instead of conventional treatments of high-dose steroid which was reported to be effective to the MS. To my knowledge, there have been no other descriptions in the literature of pathologic laughing in NMO which, and my patient is an unusual NMO case presenting with pathologic laughing and relieved with the plasmapheresis therapy.